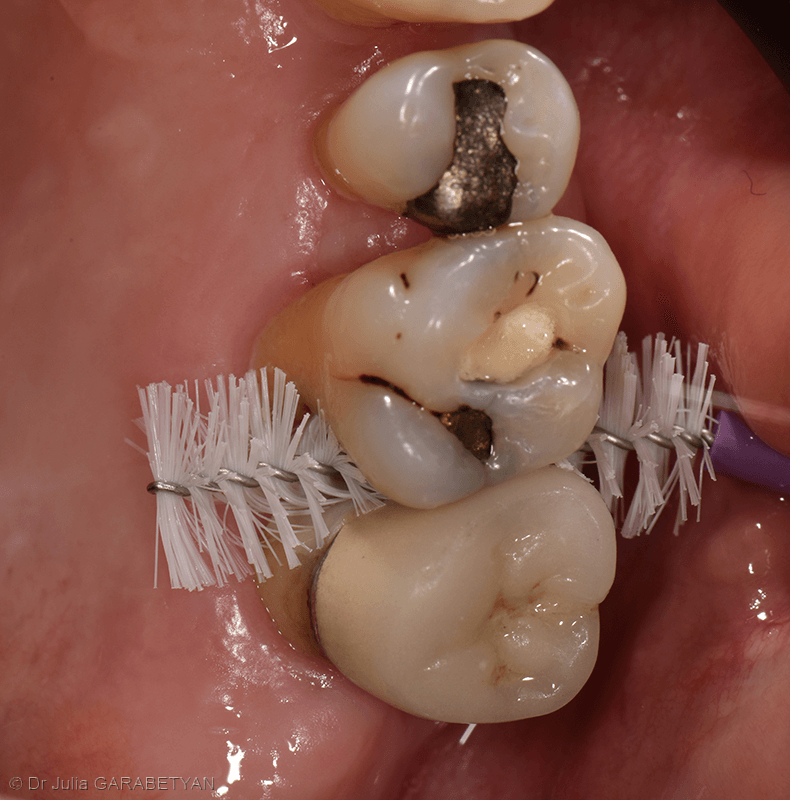
Inter-root lesions (IRLs) involve the furcation area of multi-rooted teeth and pose a therapeutic challenge due to bacterial reservoirs and complex anatomical areas, making personal plaque control and professional instrumentation difficult. The goal of this post is to understand the importance of diagnosis and prognosis in the treatment of multi-rooted teeth.

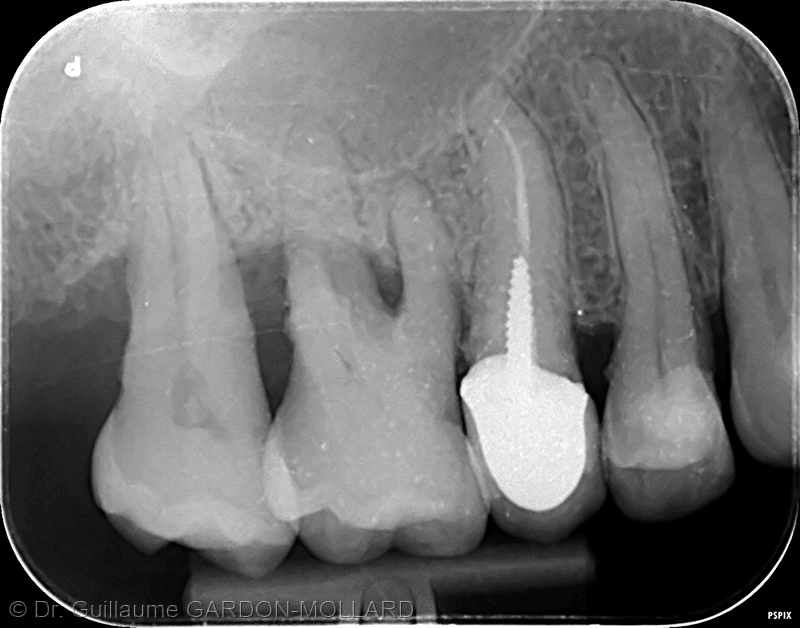
Subgingival calculus on a freshly extracted maxillary molar. Notice the significant deposits in the furcation area (Document: Dr. Guillaume Gardon-Mollard).
Diagnosis
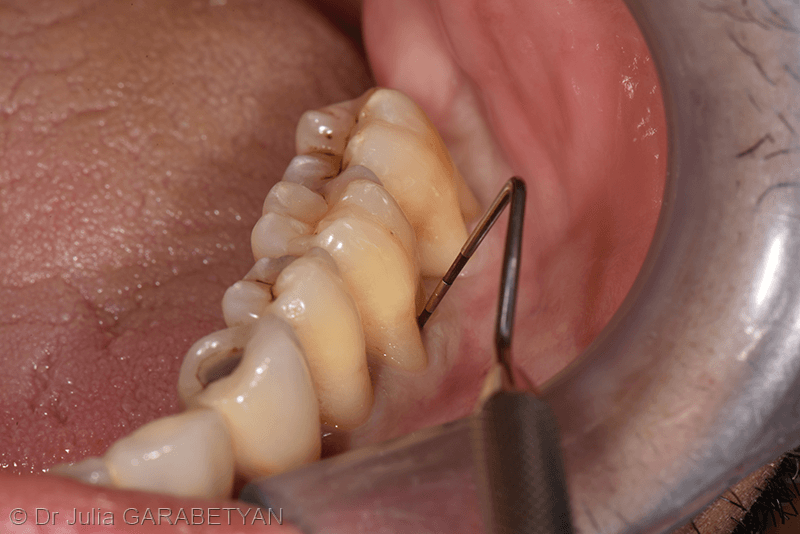
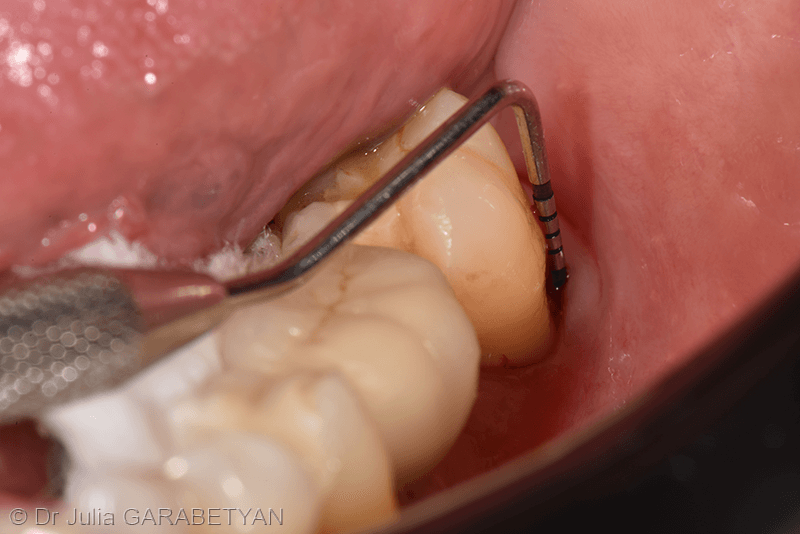
IRL diagnosis is based on periodontal probing and radiography. Clinically, an IRL is a defect characterized by two components:
1. Horizontal component, measured with a Nabers probe:
- Class I (mild): horizontal probing depth less than or equal to 3mm;
- Class II (moderate): horizontal probing depth greater than 3mm;
- Class III (severe): horizontal probing through the entire lesion.

2. Vertical component, measured with a straight periodontal probe:
- Degree A: vertical probing depth from 1 to 3mm;
- Degree B: vertical probing depth from 4 to 6mm;
- Degree C: vertical probing depth greater than or equal to 7mm.
Radiographic exams help determine the configuration of the inter-root lesion.
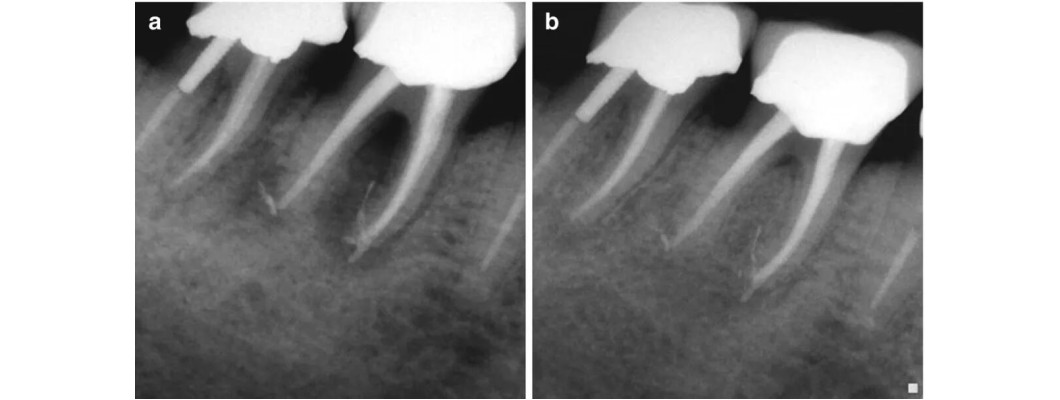
Periapical radiograph
In the maxilla, the overlapping image of the palatal root of a molar and the furcation area tends to mask the inter-root bone loss.
In the mandible, an inter-root radiolucency under the furcation is often observed with varying extents.


CBCT (Cone Beam Computed Tomography)

Prognosis
At the initial clinical examination, the presence of an IRL in multi-rooted teeth is an unfavorable prognostic factor during periodontal follow-up. This is due to the anatomical complexity (maxillary IRLs vs. mandibular IRLs), difficulty maintaining rigorous hygiene for the patient, and disinfection for the practitioner.
The prognosis primarily depends on:
- Initial severity of the IRL;
- Associated local conditions (root trunk height, furcation zone width, bone defect anatomy, associated endodontic or caries issues);
- Patient compliance with maintaining strict local hygiene;
- Periodontal treatment;
- Follow-up program and frequency.
Rigorous periodontal follow-up appears to be the most critical prognostic factor: IRL survival rates exceed 80% over follow-up periods of 8 to 22 years. However, beyond 8 years, the risk of losing molars with an IRL is higher than molars without an IRL.
The presence of a very severe IRL (horizontal and vertical components) may lead to tooth extraction from the initial phase. A tooth will only be preserved if the periodontal prognosis remains favorable throughout the follow-up.
Treatment
Traditionally, the treatment approach depends on Hamp's classification:
- Class I is treated with non-surgical options (root planing);
- Class II can be treated with conservative surgery (access flap with odontoplasty/osteoplasty, tunneling) or regenerative surgery (membrane, grafting)
The therapeutic approach for inter-root lesions (IRL) depends on the Hamp classification. The treatment options are as follows:
- Class I: Non-surgical treatment (root planing)
- Class II: Conservative surgery (access flap with odontoplasty/osteoplasty, tunneling) or regenerative surgery (membrane, grafting, amelogenin derivatives)
- Class III: Advanced resective surgery (root hemisection, amputation) or tooth extraction
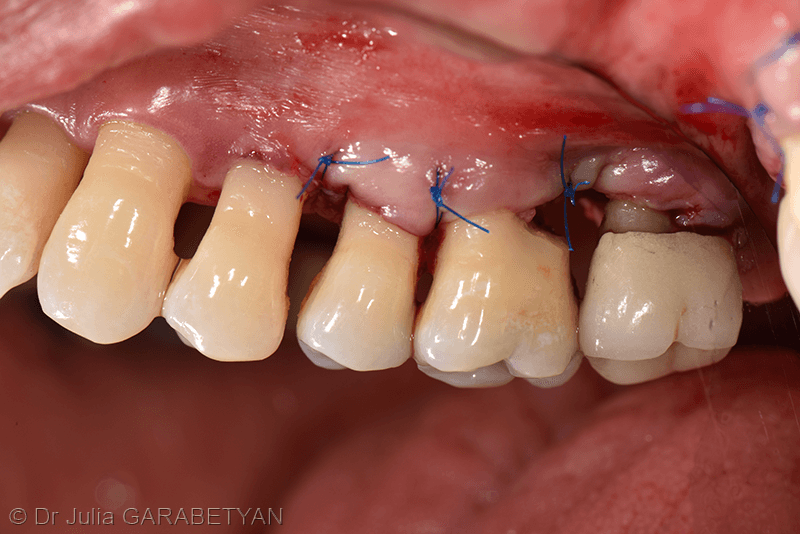
Conservative Surgery for Inter-Root Lesions
The objective of these techniques is to surgically modify the furcation anatomy of the affected tooth/teeth and facilitate access for hygiene and professional instrumentation.
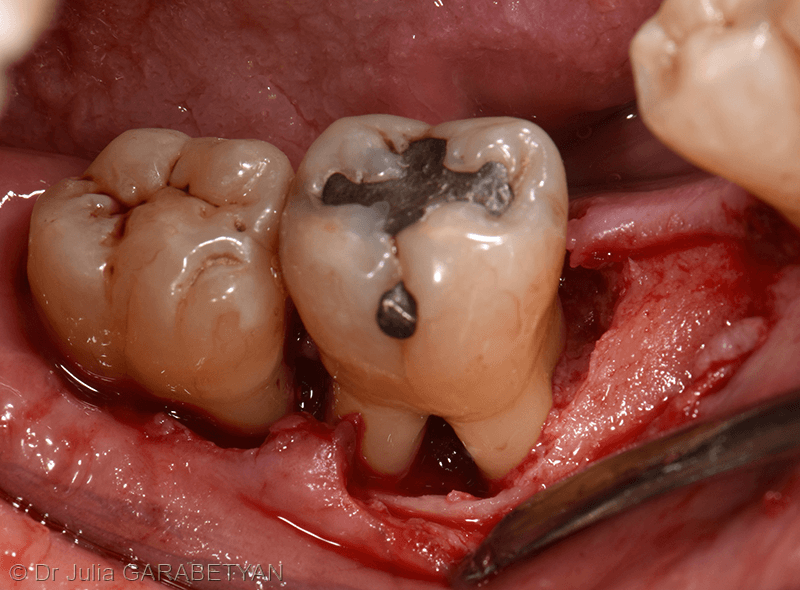
Access flap with odontoplasty/osteoplasty
Indicated for moderate IRLs when the furcation entrance can be managed by Corono-radicular reconstruction with or without osteoplasty
Survival rates are about 70% over a 12-22 year period
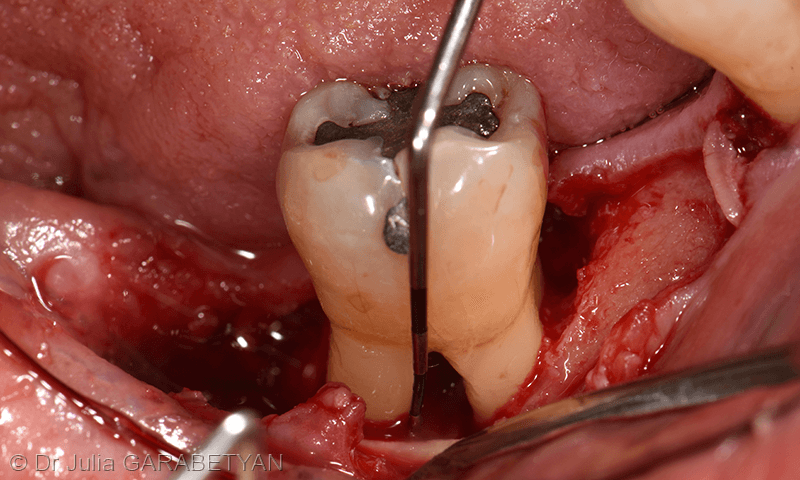
Tunneling
Indicated for moderate to severe mandibular IRLs on molars with short root trunks, long and divergent roots
Survival rates vary (around 75% at 9 years); average root caries rates are about 15.4%
Regenerative Surgery
The aim of this approach is to regenerate the destroyed inter-radicular periodontal tissues using biomaterials like amelogenin derivatives, bone substitutes, and membranes. However, IRLs respond poorly to this type of surgery. Factors to consider when choosing this approach include the stage of IRL progression, the anatomy of the bone defect, and the patient's ability to maintain a high level of oral hygiene.
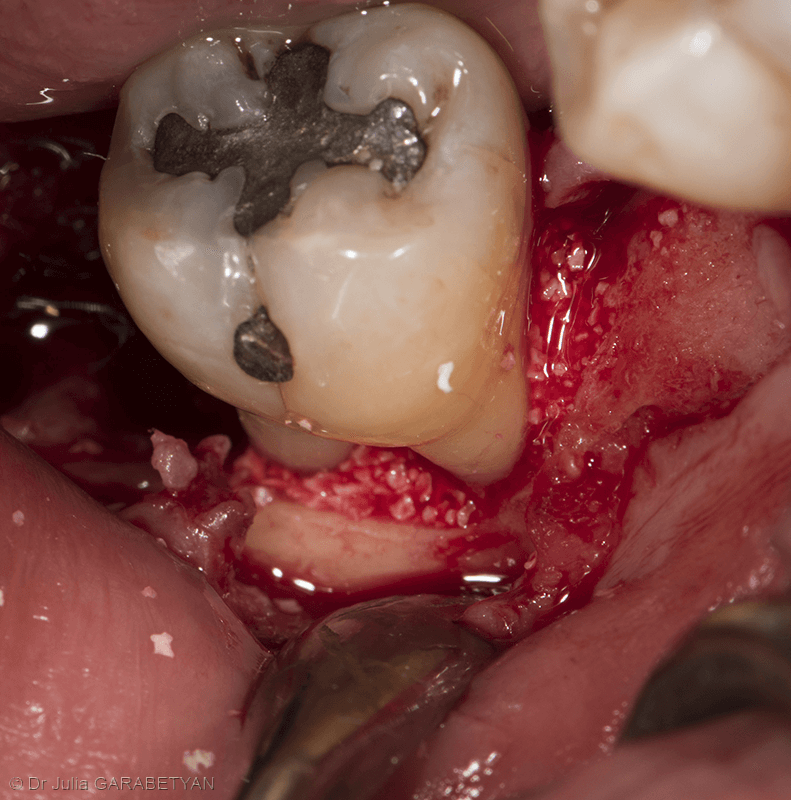
Resective Surgery
Root amputation

Technique involves removing a root while preserving the entire crown
Survival rates vary according to studies (85-100% at 5 years; 62-100% from 5-13 years)
Conclusion
The root anatomy of maxillary molars makes the prognosis of maxillary IRLs less favorable than mandibular IRLs. Treating IRLs is complex and requires a comprehensive treatment plan. Strict periodontal follow-up, dental caries prevention strategies, and proper occlusal load distribution are essential for successful treatment outcomes.
FAQs
What are the different treatment options for inter-root lesions in periodontology?
Treatment options include non-surgical treatment, conservative surgery, regenerative surgery, and resective surgery depending on the Hamp classification.
What factors should be considered when choosing regenerative surgery for inter-root lesions?
The stage of IRL progression, the anatomy of the bone defect, and the patient's ability to maintain a high level of oral hygiene should be considered.
How important is a comprehensive treatment plan for treating inter-root lesions in periodontology?
A comprehensive treatment plan is crucial as it helps address the complex nature of IRLs and ensures successful treatment outcomes.
